What is angioplasty?
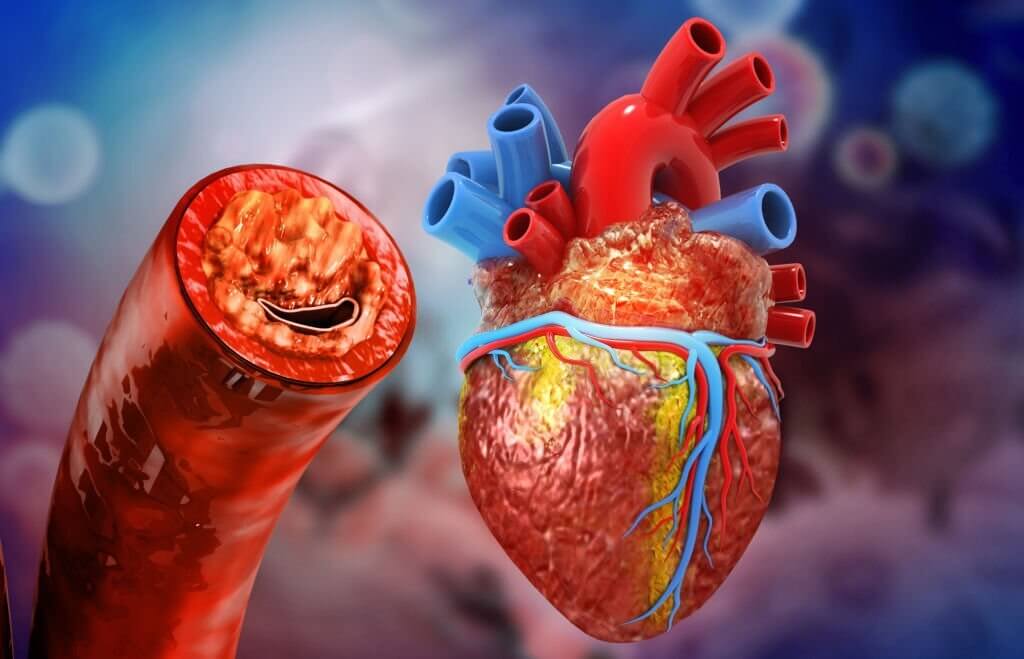
A stent is used during angioplasty to clear the blocked blood vessel. It is carried out during an angiography (angiogram), during which the doctor injects a dye into the vessels to make them visible under X-ray. Despite being the most frequently utilized, angiograms have several drawbacks. Their two-dimensional images have poor resolution. An inside look at the vessel is not possible with angiography. In addition, there is a danger that the stent will not be correctly expanded or positioned.
What is OCT?
Optical Coherence Tomography (OCT) is a modern imaging modality of cardiac conditions that gives high-resolution 3D images. It provides excellent image quality with quick pull-back speeds, procedural safety, and patient acceptability, enabling an accurate vascular lumen and stent assessment. When compared to IVUS (Intravascular Ultrasound) or conventional angiography, OCT provides unique insights into stenting procedures that might otherwise be missed1. OCT images have more than 20 times greater resolution than angiography images do. Additionally, the resolution is more than ten times higher than that of ultrasound.
When it comes to the clinical evidence for OCT, there is plenty. OCT-guided angioplasty (PCI) changed the procedure decision of treating doctors by about 90%. The use of OCT guidance was associated with reduced rates of myocardial infarctions. Furthermore, the OCT-guided procedure is better than the angiographic procedure for stent expansion.
A patient can benefit from OCT in myriads of ways. The 3D images generated by OCT help doctors customize the treatment strategy. It aids in reducing the associated risks. Having done an OCT saves the patient from undergoing unnecessary procedures or surgeries. It also empowers doctors in improving procedures and clinical outcomes.
The strategic pre-treatment approach using OCT consists of 3 main categories. They are categorized according to the degree of calcific burden: low, moderate, and high. Lipid-rich and fibrotic plaque are considered lesions with a low calcific burden. The moderate calcific burden includes mixed plaque, deep calcium, and NIH lesions. Finally, superficial calcium and calcium nodule lesions are considered as of high calcific burden. Direct stenting, semi-compliant balloon, NC and/or scoring balloon, and rotational atherectomy are used as treatment methods in the sequence of low, moderate, and high calcific burden in increasing the complexity of the treatment.
OCT image identification
There is a systematic approach for OCT image identification and treatment. When we consider the lesion, there are four factions to analyze. They are the signal, the absorption, the edges, and homogeneity. If the lesion is fibrous, it gives away bright signal-rich results whereas if it is calcific, it indicates dark signal-poor results. Regarding the Lipid lesions, they show in between the results of the previous two. The absorption can be high in lipid lesions and low in both fibrous and calcific lesions. When it comes to the edges, calcific lesions comprise sharp edges whereas fibrous and lipid lesions consist of diffuse edges. Both fibrous and lipid lesions are homogenous. On the other hand, calcific lesions are heterogeneous.
Conclusion
Cardiologists The newest intracoronary imaging method, OCT, was created to provide a clearer picture of coronary atherosclerosis and its functional impact. A high-definition view of intraluminal and endothelial features is now possible thanks to the exceptional speed and spatial resolution of modern OCT devices2.
References
- Prati F, Guagliumi G, Mintz GS, et al. Expert review document part 2: Methodology, terminology and clinical applications of optical coherence tomography for the assessment of interventional procedures. Eur Heart J. 2012;33(20). doi:10.1093/EURHEARTJ/EHS095
- Prati F, Romagnoli E, Burzotta F, et al. Clinical Impact of OCT Findings During PCI: The CLI-OPCI II Study. JACC Cardiovasc Imaging. 2015;8(11):1297-1305. doi:10.1016/J.JCMG.2015.08.013